Comprehensive Guide to Bunion Treatment: Causes, Symptoms, and Surgery Options
What is a bunion?
Bunions, or hallux valgus in doctor talk, are a gradual dislocation of your big toe joint. They stem from the way your foot functions. They are not deposits of calcium or an extra bone on the side of your foot. Bunions are more common in women than men and often present in a person’s 30-40s. How soon a bunion presents in life and how quickly it progresses is entirely determined by how the foot functions.
Bunions can cause problems in a couple ways. The bony prominence that develops on the side of your foot can get irritated by your shoes and increasing misalignment within the joint can create deep aching pain both within the joint as well as on the bottom of the joint. This can lead to swelling and difficulty finding comfortable shoes. As much as your bunion might be the focus of your attention, it is only a symptom of a bigger issue. Let’s explore why we get bunions.
So, what causes bunions?
First things first, it must be understood that the bunion is only a symptom of a more global foot mechanical issue. It is not caused by the shoes you wear, despite popular belief.
We get our foot structure from our genetics. Our foot structure will dictate function. If one of your parents has bunions, you are likely to share the same foot type and will be prone to getting them as well.
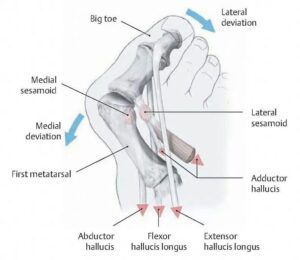
Bunions are caused by instability in the first ray of your foot. The two bones of your big toe combined with the first metatarsal bone make up this first ray. When we walk, our foot has two jobs. When the heel first strikes the ground, our foot is a mobile adapter to accommodate whatever terrain we might encounter. After heel contact, our body weight passes over the foot. At this point the foot’s job changes to a rigid lever to push us into our next step. A critical component of this rigid lever concept is that ideally the first ray forms the stiff lever that propels our momentum forward. In certain foot types however, the first ray does not become rigid and the force from the ground pushes up on the first ray which destabilizes the big toe joint. This results in the right mechanical scenario for the bunion to form. With normal alignment, the tendons and ligaments stabilize the big toe joint. However, when instability exists the tendons and ligaments become a deforming force. The first metatarsal bone deviates outward which causes the head of that bone to move out from under the big toe. While this is happening, the base of the big toe is anchored by a tendon attachment, so it loses the support of the first metatarsal under it and then falls off to the side.
At the first sign of a bunion, there exists a key opportunity. The foot function can readily be addressed with custom functional orthotics, presenting a key opportunity at the first sign of a bunion. These orthotics are in-shoe devices which control function and can stabilize the first ray, thereby preventing progression of the bunion and allowing you to avoid surgery in the future.
Likewise, transitioning to more helpful shoes with increased motion control and wider toe boxes can go a long way in providing relief. This is where your podiatrist comes in, with their extensive biomechanical knowledge, they can provide you with this solution.
How to Treat Bunions without Surgery
Treatment for bunions consists of both non-surgical and surgical options depending on your goals. If your pain is primarily bunion “bump” pain from shoe irritation, then numerous nonsurgical remedies or bunion “self-care” options are available.
These treatments can include
- changes in shoes
- stretching of shoes
- bunion shields
- bunion splints.
I want to take a minute and discuss bunion splints. There are two types: day and night. A day splint is designed to hold your big toe in better alignment while wearing your shoe. Essentially, it helps your foot fit in your shoe better. A bunion night splint is not meant to be worn with shoes. It is designed to address the bunion correctively, by pushing the metatarsal inward and pulling the big toe outward. These forces are directed to realigning the toe. Bunion night splints employ Davis’s Law of soft tissues which, simply put, says that soft tissues, like ligaments and joint capsules will adapt to stresses placed through them. This is why people stretch before athletic activity.
In conjunction to these ideas, the use of anti-inflammatory medications and physical therapy can provide an enhanced benefit. Reduction of inflammation has two distinct benefits. First, it will reduce pain, which obviously is impactful to the patient. Equally, if not more importantly, it will create the environment for the ligaments and joint capsule around the big toe joint to heal. When soft tissues (tendons, ligaments, muscle, joint capsules, etc.) are inflamed, those inflammation processed lower the pH of the tissue and create a more acidic environment which impedes the healing processes of the soft tissues. Reducing the inflammation through icing, topical anti-inflammatories or oral anti-inflammatories will restore the pH back to normal levels which allows the soft tissue to proceed with their normal healing.
Treating Bunions with Surgery
When the previously mentioned measures fail or are not indicated, surgical solutions can be explored. I divided bunion surgery into two categories: Palliative and Reconstructive.
Palliative simply means making the bunion fit better in a shoe. In this procedure the prominent head of the metatarsal is shaved down to minimize the bunion prominence and facilitate shoe wear. This in no way corrects the bunion and the rate of recurrence is very high since the bunion was never actually corrected. This procedure is best limited for a more senior individual that has bunion irritation from shoe and no longer has a propulsive heel to toe walk. For everyone else, reconstructive bunion surgery is advisable.
If your bunion hurts and the pain comes from within the joint this indicates that joint derangement is the source of the pain. In this case, reconstructive surgical intervention is warranted.
In general, there are two types of reconstructive bunion surgeries. The first being the “osteotomy” (bone cutting) procedure. In this case, the surgeon cuts the metatarsal bone into two pieces and then shifts the distal piece in ward to realign the big toe joint. The benefits of this surgery are shorter recovery time and quicker return to shoes. The downside of these types of procedures is the possibility of bunion recurrence as the procedure itself does not address the cause of the bunion. Learn more about minimal incision bunion surgery.
Alternatively, “fusion” procedures exist which do better address the cause of the bunion. In these procedures, the surgeon directs their attention to the joint behind the big toe joint which is where the metatarsal starts to deviate outward. The surgeon then realigns the metatarsal and then fuses that joint which prevents the metatarsal from ever drifting outward again. While this is a permanent bunion correction, it is associated with longer recovery, more complications and longer return to shoes.
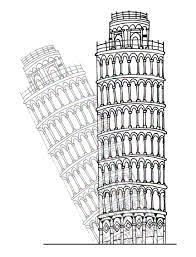
Here is the best way to look at bunion surgery: Take the Leaning Tower of Pisa and change it so that a perpendicular line can be drawn from the top and bottom. Which makes more sense – cutting it in half and shifting the top section or going to the bottom and propping it up until the structure is perpendicular to the ground?
Recovery and rehabilitation after bunion surgeries varies greatly depending on many factors: type of procedure, how the bones are held together, bone quality, smoking, and nutrition status, to name a few. The foot can be protected by a post operative shoe, walking boot, or a cast. Length of immobilization in these devices and weightbearing status is all dependent on the above-mentioned factors and your surgeon’s preference.
In summary, a bunion is a symptom of an overall foot function issue. It is a mistake to focus solely on the bunion and ignore the issue which caused it. Prompt acknowledgement and getting into a podiatrist will lead to the most positive outcome. Of course, if you ignore the bunion in the beginning, and you start noticing difficulty walking and/or pain then I implore you to seek podiatric help.
Every one of us has a particular type of foot based on structure and function. All foot types are prone to particular potential foot issues. It is always a good idea, even if you have no symptoms, to schedule an appointment with a podiatrist who can teach you about your foot type, protentional issues, and how to prevent them. You will put more miles on your feet than any vehicle that you will ever own. Understanding your feet will make sure there with you every step of the way!
To schedule a visit with Dr. Offutt at Upperline Health Richmond, click here or call 765-962-3724.
About the Author
After completing his Bachelor’s degree at Depauw University, Dr. Stephen Offutt went to Podiatry school at Barry University in Miami Shores, Florida. Despite all the sun and festivities that South Florida had to offer, he was able to earn both a master’s degree in human anatomy and my Doctorate of Podiatric Medicine after four years. The next phase of his education took me to Winona Memorial Hospital in Indianapolis where he completed his residency.
After residency, Dr. Offutt was fortunate enough to take an associate position for three years with one of his attendings. Upon completion of that term, he purchased his Richmond, IN, office from him and set up private practice for the next ten years. Towards the latter part of private practice, some of his patients began to struggle with mobility and getting out of their house. This prompted him to begin a small house call practice to compliment his office.
The creation of his modest house call practice garnered attention from a large home health care company in Indianapolis. He worked with them to further his in home care practice. From this Dr. Offutt further transitioned focus onto senior folks and became the Indiana director of podiatry for a large ancillary care company. Practicing in this world opened his eyes and mind in ways he never could have imagined. It was then that he realized the way that medicine is traditionally been taught is that doctors only intervene when someone is sick, or needs a prescription or surgery. He realized that this was not how he wanted to practice medicine. Instead, Dr. Offutt is dedicated to helping his patients live well, to avoid significant problems and focus on a more productive form of healthcare. This personal paradigm shift has led him to where he is today. Dr. Offutt is excited to return back to his Richmond office and partner with Upperline Healthcare to bring a new, comprehensive style of lower extremity wellness to Eastern Indiana.