What are Heel Spurs?

If you’ve ever stepped out of bed in the morning only to be met with a sharp, unexpected jolt of heel pain, you’re not alone and you’re definitely not imagining it.
Heel pain has a way of sneaking into your day, turning simple routines like walking to the kitchen or standing at the sink into uncomfortable challenges. For many people, that stubborn ache traces back to a common but often misunderstood condition: plantar fasciitis, often confused with or called, heel spurs.
One of the great myths is that heel spurs (those on the bottom of the heel) cause pain…they do not. Heel spurs may be small, but if traumatized, broken or jagged, they can have a big impact on how you move, work, and feel. The good news? Understanding what they are and how they develop is the first step toward finding real relief. Let’s explore what heel spurs are, why they happen, and how the right care from an Upperline Health podiatric physician can help you get back to walking comfortably again.
What exactly is a heel spur?
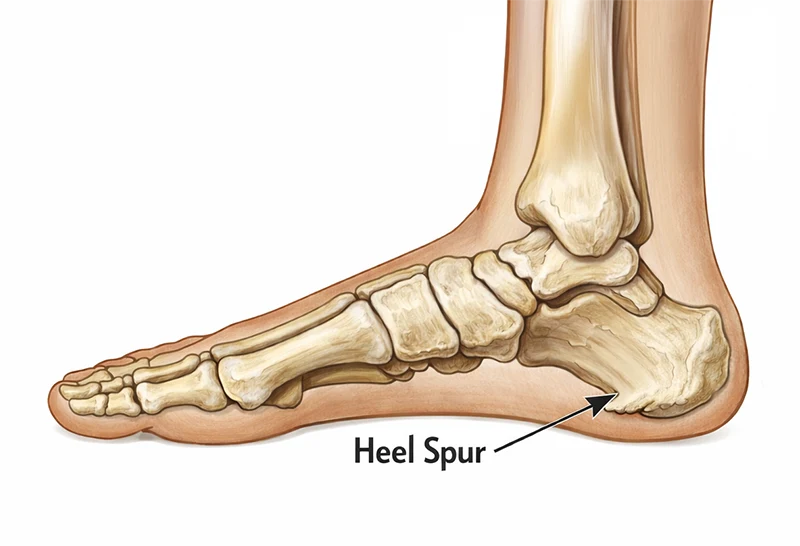
A heel spur is a small bony outgrowth on the heel bone (calcaneus). Most often, it forms on the bottom of the heel where the plantar fascia, the thick band of tissue that supports the arch, attaches. This is called a plantar calcaneal spur. Spurs can also develop on the back side of the calcaneus and those can be quite the source of pain.
Heel spurs develop gradually over time. They’re not sharp “spikes” but rather extra bone laid down in response to repeated pulling and stress at the attachment point of soft tissues. Many people with heel spurs also have plantar fasciitis, an inflammation and degeneration of the plantar fascia; and, the real cause of the pain.
Interestingly, not every heel spur causes pain. Some are found incidentally on X-rays, while others are associated with significant, chronic heel pain.
A large population study of middle-aged and older adults found that plantar heel pain affects roughly 10% of people in the general population
How do heel spurs develop?
Heel spurs form when the heel bone is exposed to repeated stress over time. Some common contributing factors include:

- Long periods of standing or walking on hard surfaces
- High-impact activities like running or jumping
- Tight calf muscles and Achilles tendon
- Flat feet or very high arches
- Excess body weight
- Poorly supportive or worn-out shoes
- Essentially, anything that stresses the plantar fascia (arch tissue) can lead to calcium deposition; a spur.
Over time, this constant pulling where the plantar fascia and other soft tissues attach to the calcaneus signals the body to lay down extra bone as a “reinforcement.” That extra bone becomes a heel spur.
Heel spurs often appear together with plantar fascia thickening and heel pain, especially in adults over 40.
How common are heel spurs and heel pain?
Heel pain is very common. A large population study of middle-aged and older adults found that plantar heel pain affects roughly 10% of people in the general population, making it one of the most frequent foot complaints seen in primary care and podiatry.
When researchers look specifically at heel spurs on X-rays, they find that they’re surprisingly common, even in people without severe symptoms. One radiographic study found plantar calcaneal spurs in about 32% of patients imaged, with higher rates in women and older adults.
How can Upperline Health podiatric physicians help with heel spurs?
At Upperline Health, our podiatric physicians focus on the whole picture of your foot and ankle health, not just the spur that shows up on an X-ray. A typical visit for heel pain or suspected heel spurs may include:
- Thorough history and exam
Your podiatric physician will ask when and where the pain occurs (first steps in the morning or after standing all day with certain shoes), what you do for work, and any sports or activities you enjoy. - Imaging when appropriate
X-rays can confirm the presence of a spur. Ultrasound or other imaging may be used in our clinics to assess the plantar fascia and surrounding soft tissue when needed. - Personalized treatment plan
Care often includes a combination of:- Targeted stretching and strengthening exercises
- Custom or prefabricated orthotics and heel cushions
- Shoe and activity modifications
- Anti-inflammatory strategies, such as ice and medications when appropriate
- Advanced options like night splints, injections, or shockwave therapy when conservative care isn’t enough
- Occasionally, the spurs in the back of the heel need to be surgically removed to obtain relief of pain
- Ongoing monitoring
Your Upperline Health podiatric physician and clinical staff track your progress over time and adjust your treatment plan to help prevent future flare-ups.
Surgery to remove a heel spur is rarely needed, and Upperline Health physicians generally reserve it for severe, persistent cases that don’t respond to comprehensive, conservative care.

Why improper management matters
Ignoring heel pain or self-treating for months with the wrong shoes or “quick fixes” can set the stage for other problems:
- Worsening or chronic plantar fasciitis
- Compensatory gait changes that strain the Achilles tendon, ankles, knees, hips, and lower back
- Higher risk of falls or instability due to altered walking patterns
- Development or worsening of conditions like lower-limb osteoarthritis, which has been linked to the presence of calcaneal spurs in some patients
The longer the heel is painful, the more the body adapts in ways that can be hard to reverse. Early evaluation and a clear treatment plan from a podiatric physician can help prevent heel pain from turning into a long-term disability.
6 ways to help prevent heel spurs
You can’t control every risk factor (like age or genetics), but you can lower your chances of developing painful heel spurs and plantar fasciitis:
1
Maintain a healthy body weight
Extra weight increases the load on your heels with every step. Even small weight reductions can lessen stress on the plantar fascia.
2
Increase activity gradually
If you’re starting a new walking or running program, build up slowly. Sudden jumps in mileage or intensity are a common setup for heel pain.
3
Choose supportive footwear
Wear shoes with good arch support, cushioning, and a slightly raised heel. Avoid very flat, unsupportive shoes and worn-out sneakers.
4
Use orthotics when recommended
Over-the-counter inserts can help distribute pressure more evenly across the foot and reduce strain on the heel.
5
Stretch your calves and plantar fascia
Regular stretching of the calf muscles and the bottom of the foot keeps tissues flexible and reduces tension at their attachment to the heel bone.
6
AVOID GOING BAREFOOT, especially first thing in the morning
Have a pair of shoes, good supportive sandals or slippers at the bedside and put them on before rising to your feet.
How to manage heel spurs if you already have them
If you’ve been diagnosed with heel spurs or suspect them based on ongoing heel pain, don’t lose hope. Many people improve with consistent, conservative care. Here are some tips from our Upperline Health podiatric clinicians:
- Work with a podiatric physician
Partnering with an Upperline Health podiatric physician ensures you have access to advanced treatments, if needed, like night splints, physical therapy, injections, and other options. Your care is coordinated and tailored to your specific needs. - Use ice and anti-inflammatory strategies
Applying ice to the heel and using appropriate anti-inflammatory medicines as advised by your Upperline Health clinician can reduce pain and swelling. - Stretch and strengthen with exercises
A physician-prescribed program to stretch your calves and plantar fascia and strengthen the small muscles of the foot can ease strain at the heel. - Wear supportive shoes and orthotics
Wearing prescribed footwear all day and using custom orthotics or heel cups can cushion the heel and support the arch.
Many people with heel spurs improve with consistent, conservative care
Take the next step: schedule with Upperline Health
If heel pain is making it hard to get through your workday, enjoy your hobbies, or simply walk around the house, you don’t have to tough it out.
Upperline Health podiatric physicians diagnose and treat heel spurs and related conditions every day, using evidence-based care to help patients reduce pain, move comfortably, and protect their long-term foot health.
Call your local Upperline Health clinic today to schedule an appointment and take the first step toward lasting relief from your heel pain.
About the Author

Dr. Garrett LaMontagne joined Upperline Health in August 2025. A native of Florida’s east coast, he earned his undergraduate degree from the University of Central Florida before receiving his Doctor of Podiatric Medicine from Kent State University College of Podiatric Medicine in 2022. He then completed a three-year Podiatric Medicine and Surgery Residency with Reconstructive Rearfoot/Ankle Surgery at Rochester General Hospital in Rochester, New York.
Dr. LaMontagne is passionate about helping patients restore function and mobility through both conservative treatments and advanced surgical care. He is committed to providing personalized, evidence-based solutions that improve quality of life.
Outside of the clinic, Dr. LaMontagne enjoys staying active by spending time outdoors, running, playing golf, and snowboarding.
Dr. LaMontagne is available for appointments at the following locations:
Upperline Health – Port Orange
790 Dunlawton Avenue
Suite C
Port Orange, Florida 32127
Upperline Health – Palm Coast
21 Hospital Drive
Suite 170A
Palm Coast, Florida 32164