Varicose Veins: They’re More Than Just Cosmetic

You may think varicose veins are just unsightly blue lines under your skin, but they’re not merely a vanity issue.
Those twisted, bulging vessels are signs of deeper problems. Ignoring them can lead to pain, swelling, skin breakdown—even serious complications that require medical attention. Often times they are “invisible”—meaning you don’t even know they exist, but you might see changes in your limb that a podiatric physician should examine.
Let’s talk about varicose veins, why you shouldn’t brush them off, and how your podiatric physician can step in and help before things get worse.
What the Research Says: 3 U.S. Studies to Know
Varicose Veins and DVT Risk
A major study in JAMA found that adults with varicose veins face significantly higher odds of developing deep vein thrombosis (DVT)—blood clots in deep veins that can be life-threatening if they travel to your lungs.1
Reduced Physical Function Among Affected Adults
A community-based U.S. cohort study discovered that older adults with varicose veins often have decreased mobility and function. The arteries may not improve, but daily aches and heaviness certainly can affect quality of life.2
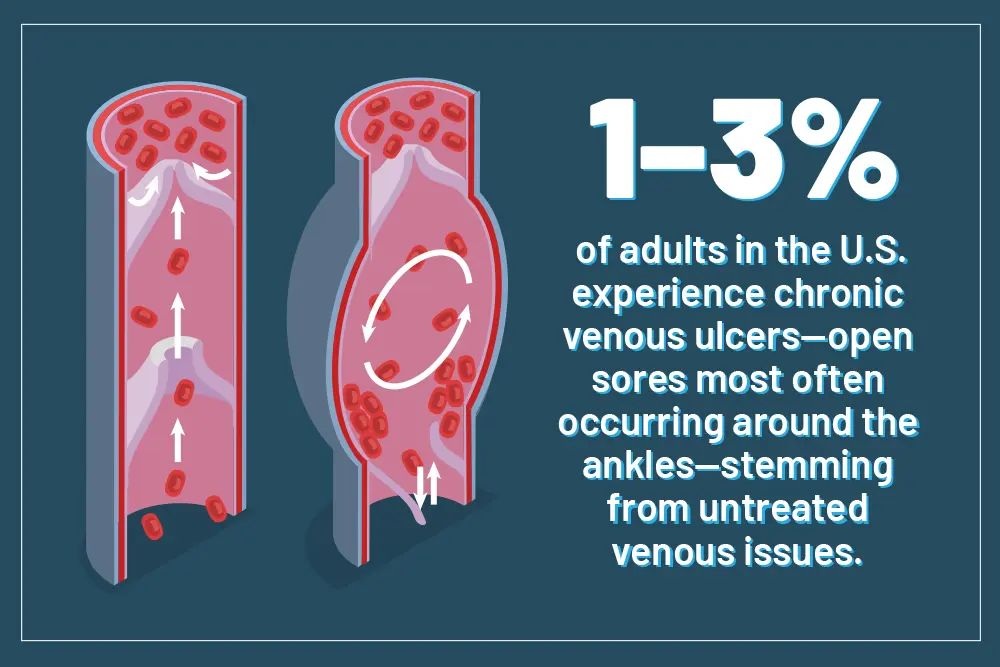
High Rates of Venous Leg Ulcers
Between 1%–3% of adults in the U.S. experience chronic venous ulcers—open sores most often occurring around the ankles or inner part of the leg—stemming from untreated venous issues.3
Three Major Issues Varicose Veins Can Cause
Blood Clots & Thrombosis (DVT)
Varicose veins are associated with a 4–5x increased risk of DVT, per observational studies.4
Why it matters:
A clot in deep veins can break free, travel to the lungs, and become a pulmonary embolism—a potentially fatal event.
Pain, Discomfort, & Activity Drop
Symptoms often include aching, heaviness, burning, cramps, and swelling—which worsen when standing or sitting. These symptoms impair mobility and contribute to inactivity, creating a harmful cycle.
Why it matters:
Reduced activity worsens overall vascular health and increases risks for obesity, diabetes, and cardiovascular disease.
Skin Damage & Venous Ulcers
Chronic pressure in the veins can lead to skin changes—pigmentation, dryness, eczema—and eventually venous leg ulcers, which are slow or impossible to heal on their own.
Why it matters:
These ulcers can become infected, extremely painful, recur frequently, and even require surgical care.
What Happens if Left Untreated?
Ignoring varicose veins sets off a cascade of worsening problems:
Stage
What Happens
Early
Mild pain/itching, visible veins, slight swelling
Progression
Worsening discomfort, pigmentation, reduced movement
Advancement
Skin thickens, eczema or phlebitis develops
Critical
Ulcers form, infections set in, bleeding or thrombosis
Each stage brings more pain, restrictions, and costs—physical and emotional.
5 Powerful Ways Upperline Health Podiatrists Can Help
Upperline Health podiatrists specialize in foot and ankle care, but they also play a vital role in vascular health including varicose veins. Here’s how:
1. Comprehensive Vascular Evaluation
Our clinical teams perform detailed physical exams and Doppler/duplex ultrasounds to assess valve function, blood flow, and possible clot danger. This helps determine the right treatment path.
2. Tailored Compression Therapy
From over-the-counter stockings to prescription-grade options, our podiatrists ensure proper fit and strength (Class II–III) for each patient. The compression from the stockings reduces pressure, eases swelling, and supports healing whether for discomfort or ulcers.
3. Lifestyle & Movement Coaching
Our clinicians give patients guidance on leg elevation, calf-strengthening exercises, sitting/standing breaks, a low-sodium diet, and weight control—all evidence-based strategies that ease symptoms and slow disease progress.
4. Coordinated Procedural Interventions
When needed, a patient will be referred for endovenous ablation (laser or radiofrequency), sclerotherapy, or phlebectomy. These minimally invasive techniques close or remove problematic veins and reduce malfunction.
5. Expert Wound & Ulcer Care
For those with ulcers or skin breakdown, our podiatrists offer debridement, advanced dressings, compression bandaging, infection monitoring, and referrals, when necessary, as an essential multidisciplinary approach.
Summary of Key Insights
Varicose veins raise the risk of blood clots, mobility decline, and venous ulcers.
U.S. studies back up these concerns with solid data on DVT, physical function, and ulcer prevalence.
Stages of varicose vein disease trend from mild discomfort to serious health risks.
Upperline Health podiatrists offer assessments, compression, exercise plans, procedural referrals, and wound care.
Everyday actions—leg elevation, movement, healthy weight, and skin monitoring—support treatment and symptom relief.
Do-It-Yourself Strategies that Make a Real Difference
Alongside podiatric care, incorporating these daily habits will help with your varicose veins:
- Elevate Your Legs – Sit with your feet above heart level for 15–30 minutes, several times a day. This activity is proven to reduce venous pressure.
- Move Regularly – Short walks, calf raises, and ankle pumps help your venous and arterial health return.
- Wear Compression Stockings – Wear during heel pressure activities like standing work, long flights, and sedentary periods.
- Maintain a Healthy Weight & Low Salt Diet – Watch your diet to reduce fluid retention and venous pressure—critical for symptom control.
- Check Skin & Symptoms – Early recognition of discoloration, eczema, ulcer signs, clots, or bleeding can prompt timely podiatric intervention.
Act Now! Don’t Wait Until It’s Too Late
Varicose veins may start out as a cosmetic concern but ignoring them is a short path to chronic pain, ulcers, clots, and even life-threatening complications.
If you’re spotting bulging veins, swelling, discomfort, or skin changes—don’t wait for them to escalate. Reach out, schedule an evaluation, and take control of your vascular health today. Your legs—and your future self—will thank you.
With Upperline Health podiatrists, you get:
- Accurate evaluation via ultrasound
- Pressure relief through compression
- Lifestyle coaching rooted in science
- Access to minimally invasive procedures
- Expert ulcer and wound management

About the Author
Dr. Andrew Green is a Board Certified foot and ankle surgeon who has been practicing with Atlantic Foot & Ankle Associates since 2002.
He is a graduate of the University of Florida and received his doctorate of podiatric medicine from Barry University School of Podiatric Medicine and Surgery in Miami Shores, Florida.
He completed an extensive three year surgical residency at Plantation General Hospital in Fort Lauderdale, Florida, with emphasis on reconstructive foot and ankle surgery, sports medicine, and diabetic foot care.
Dr. Green is available for appointments at the following location:
Upperline Health – Palm Coast
21 Hospital Drive
Suite 170A
Palm Coast, Florida 32164
References
- Batra, Dev, M.D.. “Varicose Veins & Risk of DVT: New Evidence to Consider for Providers & Patients.” Texas Vascular Institute Blog, January 30, 2023.
- Mok, Yejin, Junichi Ishigami, Yingying Sang, Anna M. Kucharska‑Newton, Maya Salameh, Jennifer A. Schrack, Priya Palta, Josef Coresh, B. Gwen Windham, Pamela L. Lutsey, Aaron R. Folsom, and Kunihiro Matsushita. 2022. “Clinically Recognized Varicose Veins and Physical Function in Older Individuals: The ARIC Study.” Journals of Gerontology, Series A: Biological Sciences and Medical Sciences 77 (8): 1637–1643.
- Bonkemeyer Millan, Susan, Run Gan, and Petra E. Townsend. “Venous Ulcers: Diagnosis and Treatment.” American Family Physician 100, no. 5 (September 1, 2019): 298–305.
- Chang, Shyue‑Luen, Yau‑Li Huang, Mei‑Ching Lee, Sindy Hu, Yen‑Chang Hsiao, Su‑Wei Chang, Chee Jen Chang, and Pei‑Chun Chen. 2018. “Association of Varicose Veins with Incident Venous Thromboembolism and Peripheral Artery Disease.” JAMA 319 (8): 807–17.