Understanding Charcot Foot: Causes, Symptoms, and the Path to Healing

Charcot foot might sound unfamiliar to many, but for people with diabetes, especially those with nerve damage in their feet, it’s a serious condition that can drastically affect mobility and quality of life.
While it can feel overwhelming, the good news is that with the right care and knowledge, including expert treatment from Upperline Health podiatrists, Charcot can be managed effectively.
Let’s break it all down – what Charcot is, who’s at risk, what symptoms to watch for, and how to manage it through movement, nutrition, and sometimes surgery.
What is Charcot Foot?
Charcot foot (also called Charcot arthropathy or neuropathic osteoarthropathy) is a progressive condition that causes weakening of the bones, joints, and soft tissues of the foot and ankle. It often starts when someone with peripheral neuropathy (nerve damage) experiences trauma or stress to the foot – and doesn’t feel the pain. As a result, they continue walking on it, which causes more damage.
Without early intervention, bones can fracture and joints can dislocate, eventually leading to a severely deformed foot.
Who is at Risk for Charcot?
People at highest risk for Charcot foot are those with diabetes who also suffer from peripheral neuropathy, which dulls pain sensations and makes injuries easier to miss. Individuals with poor blood sugar control, long-standing diabetes, or a history of foot ulcers or trauma are especially vulnerable.
Additional risk factors include obesity, kidney disease, and previous foot surgeries – all of which can contribute to poor circulation, delayed healing, and increased joint stress that set the stage for Charcot neuroarthropathy to develop.
According to a 2021 study in Diabetes Care, patients with a history of neuropathy and prior foot ulcers had the highest risk of developing Charcot (Petrova et al., 2021).
People with other conditions that impair nerve function, such as spinal cord injury, Parkinson’s disease, or multiple sclerosis, may also be at increased risk. Individuals with a sedentary lifestyle who suddenly increase their activity levels can unknowingly stress the foot, especially if neuropathy is present. In some cases, even minor foot surgeries or injuries can trigger Charcot in a vulnerable foot.
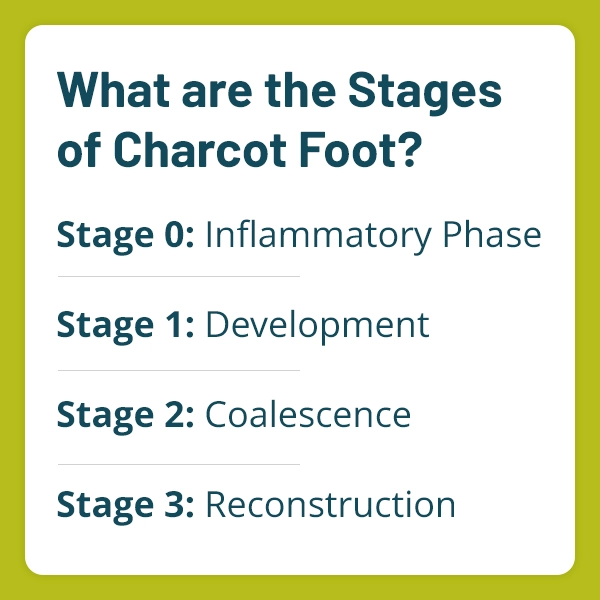
What are the Stages of Charcot Foot?
Understanding where you are in the process is key to successful treatment. Here are the 4 stages of Charcot:
- Stage 0: Inflammatory Phase
The foot may appear red, warm, and swollen, but X-rays may still look normal. This is a critical window for early detection. - Stage 1: Development
Bones weaken, fractures or dislocations occur. The arch of the foot begins to collapse. X-rays show clear changes. - Stage 2: Coalescence
The inflammation begins to subside, and the body starts repairing the damage. However, deformity becomes more apparent. - Stage 3: Reconstruction
Bones heal and reshape, but often in a misaligned way, leading to permanent structural changes and a high risk of ulcers or infections.
What are the Symptoms of Charcot Foot?
Because of the lack of sensation in the feet, early signs are often missed. But some symptoms to watch for include:
- One foot is noticeably warmer than the other
- Redness or swelling in the foot or ankle
- Sudden change in the shape of the foot
- Instability or difficulty walking
- A “rocker-bottom” foot shape
If any of these symptoms show up, especially in someone with diabetes, it’s important to see a podiatrist immediately. Don’t wait!
What are the Common Causes Charcot Foot?
Charcot foot is most often caused by a combination of:
Peripheral neuropathy
Reduces pain sensation, so injuries go unnoticed.
Repetitive trauma
Even normal walking can cause micro-injuries.
Inflammatory response
Triggers bone resorption and joint damage.
A study in the Journal of Foot and Ankle Research (Wukich et al., 2013) emphasizes the importance of early detection and intervention to prevent irreversible deformities. Without treatment, ongoing trauma leads to collapse and even the need for amputation in severe cases.
Can You Exercise with Charcot?
The short answer: yes, but very carefully.
During the early stages, especially Stages 0 and 1, complete non-weight-bearing is often necessary. That means crutches, a walker, or a wheelchair. Once healing progresses, physical activity can help maintain mobility and overall health.
Here are safe exercises to consider (with podiatrist approval):
- Seated leg lifts and ankle circles to maintain joint mobility
- Water aerobics (once cleared) for low-impact movement
- Upper body strength training to maintain muscle mass
- Resistance band exercises for gentle muscle engagement
Always follow your podiatrist’s guidance, as premature weight-bearing can worsen damage.
What Foods Should be Avoided with Charcot Foot?
Charcot is tied closely to diabetes and inflammation, so nutrition plays a role in managing the condition. Foods to limit or avoid include:
- Sugary drinks and desserts: Spikes blood sugar, worsening nerve damage
- Refined carbs (white bread, pasta): Inflammatory and increase insulin resistance
- Processed meats: Contain preservatives that can promote inflammation
- Fried foods and trans fats: Inflammatory and harmful for cardiovascular health
Instead, opt for an anti-inflammatory, blood sugar-friendly diet with lean proteins, whole grains, healthy fats (like omega-3s), and plenty of colorful vegetables.
Staying hydrated, eating on a consistent schedule, and incorporating foods rich in calcium and vitamin D (such as leafy greens and low-fat dairy) can also support bone health and healing. Limiting alcohol intake is equally important, as it can interfere with blood sugar regulation and nutrient absorption.
What are the Complications of Charcot Foot?
If untreated, Charcot can result in severe deformities, ulcers, infections, and even amputation. According to Rogers et al. (2011) in The Journal of the American Podiatric Medical Association, one of the greatest challenges in managing Charcot is the delayed diagnosis due to the subtle nature of early symptoms.
Other complications include:
- Chronic foot ulcers
- Skin and bone infections
- Loss of function or mobility
- Psychological stress from lifestyle changes
Because Charcot can cause the foot to collapse into an unstable shape, patients are also at risk for ankle sprains and falls. Long-term use of offloading devices like boots or braces, while necessary, can also contribute to muscle atrophy if not monitored closely. That’s why comprehensive care from a team that understands the full scope of the condition is critical.
Why Choose Upperline Health for Charcot Treatment?
When it comes to treating Charcot foot, experience matters. Our Upperline Health podiatrists use advanced tools and techniques to identify Charcot early and guide patients through every phase of healing.
If necessary, I offer minimally invasive surgical techniques designed to correct deformities, preserve function, and prevent further damage. The MIS (Minimally Invasive Surgery) Charcot procedure is a specialized technique used to correct deformities caused by Charcot neuroarthropathy with minimal disruption to surrounding tissues.
Through small incisions, I can realign bones, stabilize joints, and remove damaged tissue using advanced instruments and imaging. This approach reduces recovery time, lowers the risk of infection, and preserves more of the foot’s natural structure compared to traditional open surgery. It’s particularly effective for patients with diabetes, helping to prevent ulcers and reduce the risk of amputation.
When you work with our clinics, you’ll benefit from:
- Early diagnosis through in-depth foot evaluations
- Customized bracing and off-loading devices to protect the foot
- Coordination with diabetes care teams
- Surgical intervention (when necessary) using advanced MIS techniques
- Long-term planning to prevent recurrence
Charcot may be progressive, but with the right podiatric care, it doesn’t have to control your life.
Final Thoughts
Charcot foot is a serious condition, but it’s not a life sentence. With early detection, thoughtful care, and support from experts like the team at Upperline Health, people living with Charcot can stay mobile, active, and optimistic.
If you or someone you know has diabetes and is experiencing foot changes, don’t wait. Talk to a podiatrist today – because when it comes to Charcot, time really is of the essence.
References:
- Petrova, N. L., et al. (2021). “Risk factors and management of Charcot neuroarthropathy in diabetes.” Diabetes Care.
- Wukich, D. K., et al. (2013). “Diabetic Charcot foot: current concepts and review.” Journal of Foot and Ankle Research.
- Rogers, L. C., et al. (2011). “The Charcot foot in diabetes.” Journal of the American Podiatric Medical Association.